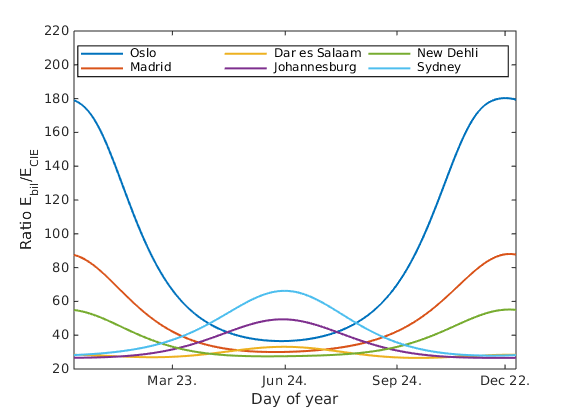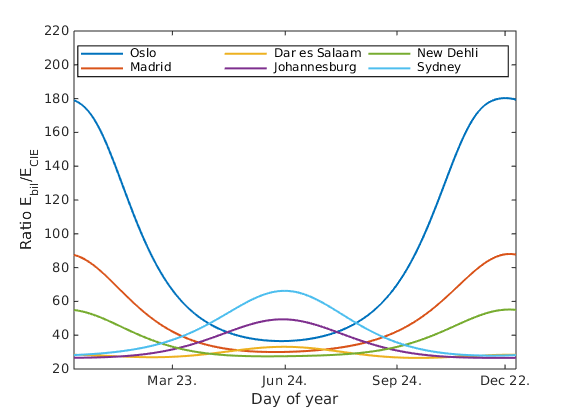
To investigate how solar zenith angle changes with geographical location and time of year, the incoming irradiance in six selected locations were simulated at noon in the local time zone for each day of 2015. The locations were Oslo, Madrid, Dar es Salaam, Johannesburg, New Delhi and Sydney. The resulting ratio of beneficial to harmful weighted irradiation is shown in figure 2. All ratios have the same overall shape, which results from the optical properties of the atmosphere. The ratio of beneficial to harmful irradiation is larger for less transparent atmospheric conditions, however, the irradiation is much stronger for more transparent conditions.
Figure 2: Ratio of Ebil=ECIE asfunction of
geographical location and time of year.
There is a trade-off between a more beneficial ratio of irradiation and high values of irradiation. If the infants were to be treated in the afternoon, when the ratio is highest, they would have to be exposed for a longer timespan than in the middle of the day. An inclined position towards the sun may however decrease the exposure time. The ratio also suggests that the treatment might be more predictable when the solar zenith angle is below 30°, as the ratio is stable for these angles. However, more research is needed to estimate required exposure times for sufficient treatment of neonatal jaundice by solar exposure, and the accompanying health risks. To avoid adverse skin effects from exposure to UV radiation, it is important that the absorbed dose in the infants at all times stay below the minimal erythema dose.
The project concludes that using sunlight as a method of treatment for neonatal jaundice is possible, especially in locations with abundant and stable access to sunlight. Further research includes a comparison with current treatment standards with respect to exposure time, and a modelling of the exact effect of blue light on the bilirubin molecules in infant skin. The atmospheric conditions will also be developed to simulate actual conditions for selected areas related to low-income countries where this method of treatment is more relevant.
[1] B.O. Olusanya, T.A. Ogunlesi, P. Kumar, N.Y. Boo, I.F. Iskander, M.F.B de lmeida, Y.E. Vaucher, T.M. Slusher, “Management of late-preterm and term infants with hyperbilirubinaemia in resource-constrained settings”,BMC Pediatrics.15(39) (2015).
[2] The International Commision on Non-Ionizing Radiation Protection, “ICNIRP Guidelines on limits of exposure to ultraviolet radiation of wavelengths between 180 nm and 400 nm (incoherent optical radiation)”, Health Physics 87(2), 171–186 (2004).
[3] B. Mayer, A. Kylling, C. Emde, R. Buras, U. Hamann, J. Gasteiger, B, Richter, “libRadtran User’s Guide”, http://www.libradtran.org/doc/libradtran.pdf (2015).
[4] A.A. Lamola, M. Russo, “Fluoresence excitation spectrum of bilirubin in blood: A model for the action spectrum for phototherapy of neonatal jaundice”, photochemistry and Photobiology. 90(2) 294–296 (2014).
[5] Commission Internationale de L’Eclairage, “Erythema Reference Action Spectrum and Standard Erythema Dose, ISO 17166:1999/CIE S 007-1998”, (Vienna: CIE) (1999).